ANNAPOLIS (Feb. 15, 2018)—One more day without treatment for a person struggling with opioids—as a Maryland delegate, a recovery expert and parents of children mired in addiction have said—could be the difference between life and death.
A relatively recent spike in deaths related to the synthetic opioid fentanyl, its cousin carfentanil and ever-emerging variations of the two has emphasized the importance of getting addicts into treatment immediately, said Delegate Nic Kipke, R-Anne Arundel.
That's why Kipke, the Maryland House minority leader, is sponsoring a bill granting parents of adults struggling with addiction more authority to act on their children's behalf.
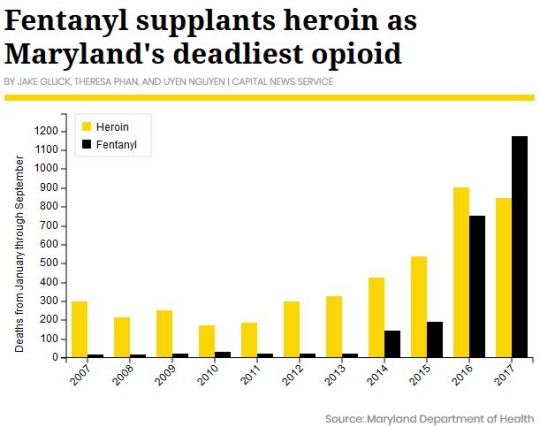
Fentanyl has overtaken heroin as the deadliest drug in Maryland. Statewide, deaths related to fentanyl surged from 192 over the first three quarters of 2015, to 1,173 fatalities over the same period in 2017—a 510 percent increase, Maryland health department data show.
Carfentanil—a drug commonly used to sedate elephants—also continued its emergence. There were 57 carfentanil-related deaths statewide over the first nine months of 2017 compared to zero over the previous two years, according to the state health agency.
Fentanyl is 50 times stronger than heroin; carfentanil is 5,000 times more potent than heroin, according to the U.S. Drug Enforcement Administration.
Fentanyl "can be lethal in the 2-milligram range," the DEA says, while the lethal range for carfentanil is uncertain, but minute.
Considering the potency of the drugs, which are often created in clandestine laboratories in China and Mexico, "this is a different kind of addiction, a different problem," Kipke told the University of Maryland's Capital News Service.
His 2018 bill would allow parents or guardians of adult children—who must be dependent through health insurance—to involuntarily admit their child to an in-patient treatment facility. Kipke introduced then withdrew the same bill during the 2017 General Assembly session after the House Health and Government Operations Committee delivered an unfavorable report on it.
The person must "not be a minor," must have "experienced a drug overdose" and have "health insurance coverage as a dependent under the individual's parent's" plan, according to a fiscal and policy note for the 2017 bill.
"What I'm seeking to do is provide parents of children who are still dependent … an opportunity to interrupt their child's addiction," Kipke said.
The Maryland State Medical Society, MedChi, agrees with Kipke that the scale of the opioid epidemic warrants new tools, said Gene Ransom, the organization's chief executive officer.
"Given that we're in a crisis," Ransom said, there needs to be more options to get people into treatment. "Giving parents another tool to help solve the problem is a no-brainer."
Survivors' perspectives
Carin Miller, president and co-founder of Maryland Heroin Awareness Advocates, said that her oldest son started using then abusing Percocet—a common opioid painkiller—in his early 20s, developing an addiction before turning to heroin.
"It was frustrating and heartbreaking when you see your son so sick and gray and on death's door," she said. "As a mother, when your child is sick or hurt … you always work your hardest to make them better."
"But when they're addicted," Miller said, "you can't."
Kipke is concerned for many of his constituents, many of whom have asked him for a tool to help their children, he said.
This year there were 108 opioid-related overdoses in Anne Arundel County through Feb. 8, compared to 113 through the same date a year prior, according to county police data.
But 18 of the 108 overdoses resulted in death—a 100 percent increase over the nine fatalities through the same date in 2017.
Over the first nine months of 2017, the county recorded 145 fatal opioid-related overdoses, a 12 percent increase over January-September of 2016, state data show.
A non-fatal overdose can be an important opportunity for intervention, experts say, but in Maryland and other states, those who are hospitalized because of overdoses can sign themselves out.
"If somebody who needs Narcan because they just overdosed, they need to be committed," Miller said.
Narcan is a brand name of the overdose-reversing opioid antagonist, naloxone. All first responders in Maryland are equipped with a form of the life-saving drug, which comes in a nasal spray form.
Miller, a Frederick County, Maryland, resident said these kind of tools weren't available to her as a mother throughout her son's struggle with addiction. Had involuntary admission been an option, Miller said she "most certainly would have" utilized the authority to admit her son.
"I would've done anything in the world to save my son," she added.
Pasadena, Maryland, native Rob Snead, 24, said he's been clean for seven months after using and abusing drugs for a decade. He has overdosed.
"When you come to, you're in withdrawal," he said. "And the only thing you can think about is getting yourself in a position to get well again."
Snead said that in the moment, addicts "don't care about seeking the accurate help, they think about what they can do immediately to feel better."
Snead described withdrawal from opioids as "overwhelming" and "a miserable state of being," and said that often the quickest way to feel better was to score more drugs and to take them.
Treatment community divided
It's been said that an addict must be ready for treatment in order for it to be successful, a notion Kipke acknowledged.
But that line of thinking could be outdated.
"If we continue to look at it like they're not ready," Miller said. "There are some that will never be ready."
Dr. Sally Satel, a resident scholar at the American Enterprise Institute who works part time in a methadone clinic in Washington, said the idea that addicts must be ready for treatment is "so wrong," and called it "one of the many cliches" surrounding the opioid crisis.
"Why do you think drug courts work?" she said.
But other addiction treatment experts have concerns about the practicality, effectiveness and safety of involuntary commitment.
"You really can't force someone to participate in treatment if they don't want to," said Vickie Walters, executive director of the Baltimore-based REACH substance abuse treatment program at the Institutes for Behavior Resources.
Getting an assessment of a patient is always important, but that if that patient was forced, Walters said, "it's tough to get good information."
Howard Ashkin, president of the Maryland Association for the Treatment of Opioid Dependence, said he worries that involuntary commitment could lead to a litany of problems.
"I've never read anything that has borne out any good outcomes," of forced treatment, Ashkin said. "I don't envision good outcomes."
Involuntary admission could make some of the adult children angrier, he said.
Ashkin said he worries that addicts will go along with the treatment, then go out to use again. But their tolerance will have diminished, he said, which increases the odds of overdose and possibly death.
Involuntary treatment programs, like drug court, Satel said, often work because it gives the individual a chance to take a step back to think about their situation and "internalize the values of the program."
Involuntary admittance could lead the individual to resent the family member who mandated their admission, Ashkin said.
Ashkin and Walters said they aren't convinced that it's worth the risk. Addicts rarely recover successfully their first time through treatment, and about 40 percent to 60 percent relapse, according to the National Institute on Drug Abuse.
Forcing an addict to get help could "leave a bad taste in (their) mouth about treatment," discouraging them from seeking treatment in the future, Walters said.
Both Ashkin and Walters were concerned about whether treatment facilities around the state were capable of or ready to admit involuntarily committed patients.
"The court will only order this type of thing if there is a bed for the individual," Kipke said.
"Are there enough beds? No," the delegate said. But they're becoming "increasingly available as this problem is getting support and funding from the government."
Is this bill the answer?
More than 30 other states have enacted similar statutes that allow for the involuntary commitment of adults for substance abuse, according to the Journal of the American Academy of Psychiatry and the Law.
Massachusetts is one such state, and its "system has become an unintended mechanism for getting people into treatment," said Leo Beletsky, associate professor of law and health sciences at the Northeastern University School of Law. In many ways the statute "was designed to be a system of last resort."
Massachusetts has been using prisons as treatment facilities for those who are involuntarily committed, Beletsky said. Many of the patients' treatment is un-medicated, increasing the risk for overdose and death after treatment, according to Beletsky.
The law professor said that putting somebody into treatment without their consent is "fundamentally un-American," and that the Massachusetts policy "basically fails" from the perspective of health and civil liberties.
"Evaluating what other states have done was extensively considered and we're open to any other suggestions as to how we could gain the support of the legislature to enact a reasonable policy, like this," Kipke said.
Snead said that Kipke's bill "has the potential to be very beneficial to people," but that success varies depending on the individual—treatment works differently for everybody.
Self-described as stubborn, Snead said that for him, the decision to get clean had to come from within.
"I had to decide myself. I had to decide that I was done," he said.
But, he said, he understands the standpoint behind his delegate's bill, as "a lot of parents are losing their kids."
Through her organization, Miller hosts family peer support groups in Frederick County. She's heard many heart-wrenching stories, some from parents who weren't able to save their children "from this dark path to death."
Miller's son is alive, but she lost him for the six years of his life that were "hijacked by heroin." Now, she said, he lives in another state, away from temptation and connections back home.
He's "a good man who has a bad disease," she said.
She supports Kipke's bill because she doesn't want other parents to feel like she did, "Like you're a failure as a mother because you can't make (your child) better."


